Periodontal Disease
Periodontal Disease
What is Periodontal (Gum) Disease?
Stages & Types of Periodontal Disease
Signs & Symptoms of Periodontal Disease
Diagnosis of Periodontal Disease
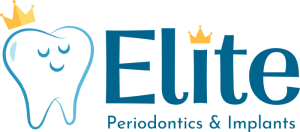
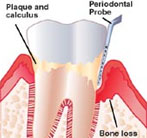
 The word periodontal means “around the tooth”. Periodontal disease attacks the gums and the bone that support the teeth. Plaque is a sticky film of food debris, bacteria, and saliva. If plaque is not removed, it turns into calculus (tartar). When plaque and calculus are not removed, they begin to destroy the gums and bone. Periodontal disease is characterized by red, swollen, and bleeding gums.
The word periodontal means “around the tooth”. Periodontal disease attacks the gums and the bone that support the teeth. Plaque is a sticky film of food debris, bacteria, and saliva. If plaque is not removed, it turns into calculus (tartar). When plaque and calculus are not removed, they begin to destroy the gums and bone. Periodontal disease is characterized by red, swollen, and bleeding gums.
Four out of five people have periodontal disease and don’t know it! Most people are not aware of it because the disease is usually painless in the early stages.
Not only is it the number one reason for tooth loss, research suggests that there may be a link between periodontal disease and other diseases such as, stroke, bacterial pneumonia, diabetes, cardiovascular disease, and increased risk during pregnancy. Researchers are determining if inflammation and bacteria associated with periodontal disease affects these systemic diseases and conditions. Smoking also increases the risk of periodontal disease.
Good oral hygiene, a balanced diet, and regular dental visits can help reduce your risk of developing periodontal disease.
What is Periodontal (Gum) Disease?
 The term “periodontal” means “around the tooth.” Periodontal disease (also known as periodontitis and gum disease) is a common inflammatory condition which affects the supporting and surrounding soft tissues of the tooth; also the jawbone itself when in its most advanced stages.
The term “periodontal” means “around the tooth.” Periodontal disease (also known as periodontitis and gum disease) is a common inflammatory condition which affects the supporting and surrounding soft tissues of the tooth; also the jawbone itself when in its most advanced stages.
Periodontal disease is most often preceded by gingivitis which is a bacterial infection of the gum tissue. A bacterial infection affects the gums when the toxins contained in plaque begin to irritate and inflame the gum tissues. Once this bacterial infection colonizes in the gum pockets between the teeth, it becomes much more difficult to remove and treat. Periodontal disease is a progressive condition that eventually leads to the destruction of the connective tissue and jawbone. If left untreated, it can lead to shifting teeth, loose teeth and eventually tooth loss.
This calculus, or tartar, cannot be removed by brushing and flossing, and must be dislodged by a dental professional.
Stages & Types of Periodontal Disease
Periodontal disease is the leading cause of tooth loss among adults in the developed world and should always be promptly treated.
Stages of Periodontal Disease
Periodontal disease (also known as periodontitis and gum disease) is a progressive disease which affects the supporting and surrounding tissue of the gums, and also the underlying jawbone. If left untreated, periodontal disease can result in loose, unstable teeth, and even tooth loss. Periodontal disease is in fact the leading cause of tooth loss in adults in the developed world and should not be taken lightly.
Periodontal disease begins when the toxins found in plaque start to attack the soft or gingival tissue surrounding the teeth. This bacterium embeds itself in the gum and rapidly breeds, causing a bacterial infection. As the infection progresses, it starts to burrow deeper into the tissue causing inflammation or irritation between the teeth and gums. The response of the body is to destroy the infected tissue, which is why the gums appear to recede. The resulting pockets between the teeth deepen and, if no treatment is sought, the tissue which makes up the jawbone also recedes causing unstable teeth and tooth loss.
Types of Periodontal Disease
There are many different varieties of periodontal disease, and many ways in which these variations manifest themselves. All require immediate treatment by a periodontist to halt the progression and save the gum tissue and bone. Here are some of the most common types of periodontal disease along with the treatments typically performed to correct them:
Gingivitis
 Gingivitis is the mildest and most common form of periodontitis. It is caused by the toxins in plaque and leads to periodontal disease. People at increased risk of developing gingivitis include pregnant women, women taking birth control pills, people with uncontrolled diabetes, steroid users and people who control seizures and blood pressure using medication.
Gingivitis is the mildest and most common form of periodontitis. It is caused by the toxins in plaque and leads to periodontal disease. People at increased risk of developing gingivitis include pregnant women, women taking birth control pills, people with uncontrolled diabetes, steroid users and people who control seizures and blood pressure using medication.
Treatment: Gingivitis is easily reversible using a solid combination of home care and professional cleaning. The dentist may perform root planing and deep scaling procedures to cleanse the pockets of debris. A combination of antibiotics and medicated mouthwashes may be used to kill any remaining bacteria and promote the good healing of the pockets.
Chronic Periodontal Disease
Chronic periodontal disease is the most common form of the disease, and occurs much more frequently in people over 45. Chronic periodontal disease is characterized by inflammation below the gum line and the progressive destruction of the gingival and bone tissue. It may appear that the teeth are gradually growing in length, but in actuality the gums are gradually recessing
 |
 |
Treatment: Unfortunately unlike gingivitis, chronic periodontal disease cannot be completely cured because the supportive tissue cannot be rebuilt. However, the dentist can halt the progression of the disease using scaling and root planing procedures in combination with antimicrobial treatments. If necessary, the periodontist can perform surgical treatments such as pocket reduction surgery and also tissue grafts to strengthen the bone and improve the aesthetic appearance of the oral cavity.
Aggressive Periodontal Disease
Aggressive periodontal disease is characterized by the rapid loss of gum attachment, the rapid loss of bone tissue and familial aggregation. The disease itself is essentially the same as chronic periodontitis but the progression is much faster. Smokers and those with a family history of this disease are at an increased risk of developing aggressive periodontitis.
Treatment: The treatments for aggressive periodontal disease are the same as those for chronic periodontal disease, but aggressive periodontal disease sufferers are far more likely to require a surgical intervention. This form of the disease is harder to halt and treat, but the dentist will perform scaling, root planing, antimicrobial, and in some cases laser procedures in an attempt to save valuable tissue and bone.
Periodontal Disease Relating to Systemic Conditions
Periodontal disease can be a symptom of a disease or condition affecting the rest of the body. Depending on the underlying condition, the disease can behave like aggressive periodontal disease, working quickly to destroy tissue. Heart disease, diabetes and respiratory disease are the most common cofactors, though there are many others. Even in cases where little plaque coats the teeth, many medical conditions intensify and accelerate the progression of periodontal disease.
Treatment: Initially, the medical condition which caused the onset of periodontal disease must be controlled. The dentist will halt the progression of the disease using the same treatments used for controlling aggressive and chronic periodontal disease.
Necrotizing Periodontal Disease
This form of the disease rapidly worsens and is more prevalent among people who suffer from HIV, immunosuppression, malnutrition, chronic stress or choose to smoke. Tissue death (necrosis) frequently affects the periodontal ligament, gingival tissues and alveolar bone.
Treatment: Necrotizing periodontal disease is extremely rare. Because it may be associated with HIV or another serious medical condition, it is likely the dentist will consult with a physician before commencing treatment. Scaling, root planing, antibiotic pills, medicated mouth wash and fungicidal medicines are generally used to treat this form of the disease.
If you have any question or concerns about the different types of periodontal disease and treatments, please ask your dentist.
Signs & Symptoms of Periodontal Disease
Periodontal disease (also known as periodontitis and gum disease) is a progressive condition and the leading cause of tooth loss amongst adults in the developed world. Periodontal disease occurs when the toxins found in plaque begin to irritate or inflame the gingiva (gum tissue). The resulting bacterial infection often known as gingivitis, can eventually lead to the destruction of the gum tissue and underlying bone. If periodontal disease is not treated, it can also lead to loose teeth or tooth loss.
There are many common types of periodontal disease including aggressive, chronic, necrotizing periodontitis, and periodontitis associated with systemic diseases. Each of these types of periodontal disease has its own distinct characteristics and symptoms, and all require prompt treatment by a dentist to halt subsequent bone and tissue loss.
Common Signs & Symptoms
It is extremely important to note that periodontal disease can progress without any signs or symptoms such as pain. This is why regular dental checkups are exceptionally important. Described below are some of the most common signs and symptoms of periodontitis.If you have any of these signs or symptoms, the advice of a general dentist or periodontist should be sought as soon as possible:
Unexplained bleeding– Bleeding when brushing, flossing or eating food is one of the most common symptoms of a periodontal infection. The toxins in plaque cause a bacterial infection which makes the tissues prone to bleeding.
Pain, redness or swelling– A periodontal infection may be present if the gums are swollen, red or painful for no apparent reason. It is essential to halt the progression of the infection before the gum tissue and jaw bone have been affected. It is also critical to treat the infection before it is carried into the bloodstream to other areas of the body.
 |
 |
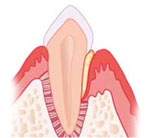
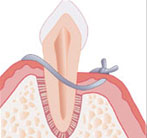
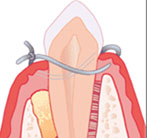
| Plaque causing inflamed gums and gingivitis | Gingivitis with calculus seen between teeth |
Longer-looking teeth – Periodontal disease can lead to gum recession. The toxins produced by bacteria can destroy the supporting tissue and bones, thus making the teeth look longer and the smile appear more “toothy.”
Bad breath/halitosis– Although breath odor can originate from back of the tongue, the lungs and stomach, from the food we consume, or from tobacco use, bad breath may be caused by old food particles which sit between the teeth and underneath the gum line. The deeper gum pockets are able to house more debris and bacteria, causing a foul odor.
Loose teeth/change in bite pattern– A sign of rapidly progressing periodontitis is the loosening or shifting of the teeth in the affected area. As the bone tissue gets destroyed, teeth that were once firmly attached to the jawbone become loose or may shift in position.
Pus – Pus oozing from between the teeth is a definitive sign that a periodontal infection is in progress. The pus is a result of the body trying to fight the bacterial infection.
If you have any further questions about the signs and symptoms of periodontal disease, please ask your dentist.
Diagnosis of Periodontal Disease
Dental/Medical Histories
Health Considerations
Clinical Examination
Dental Radiographs (X-RAYS)
Diagnosis
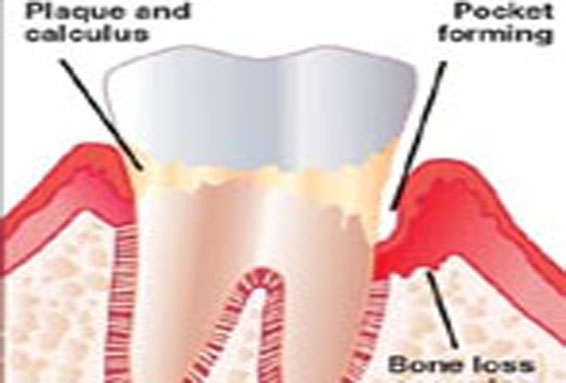
Before any periodontal treatment is undertaken, a diagnosis must be made. To reach a diagnosis, the patient’s dental and medical histories must be taken, a clinical examination must be performed, and dental x-rays (radiographs) must be reviewed. These steps are generally accomplished during the initial consultation appointment, although a second consultation appointment may be needed, particularly when additional information must be obtained.
 |
 |
 |
|
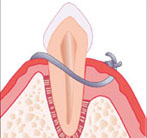
Periodontal probe ready to measure pocket |
Probe inserted 5mm under gum to base of pocket |
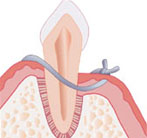
Probe held beside gum to visualize depth of pocket |
Dental / Medical Histories
For decades we have known that a prime indicator for future periodontal breakdown is a past history of periodontal disease. By taking a dental history and evaluating previous x-rays, we have a better understanding about the rate of disease progression, and can determine what must be done to prevent further breakdown. In the last decade periodontists have also begun to understand that periodontal disease is a result of bacteria interacting with the patient’s defense systems. How the patient’s body responds to the bacterial (plaque) assault depends on the “host” resistance. Some people are fortunate, and have minor periodontal disease even with poor oral hygiene. For others, the same amount of bacteria may cause advanced periodontal disease and bone loss.
In other words, certain patients are very susceptible to periodontal disease, and these patients must be particularly diligent with their oral hygiene and maintenance to reduce the bacteria challenge. By taking a complete Medical History we can determine if the patient has certain risk factors and may modify treatment accordingly
Health Considerations
- Smoking – A host factor that CAN be altered, and one that GREATLY increases the risk of disease.
- Diabetes– Increases the risk of disease if not well controlled.
- Stress – Long-term stress may adversely alter the way we fight periodontal disease.
- Hormones – Increases in gingival inflammation is seen with increased levels of estrogen.
- Medication – Many drugs including oral contraceptive pills, heart medicines, anti-depressants and steroids affect the overall condition of teeth and gums; making them more susceptible to gum disease. Steroid use promotes gingival overgrowth, which makes swelling more commonplace and allows bacteria to colonize more readily in the gum tissue.
- Severe Osteopenia– May result in more jawbone loss, particularly in postmenopausal women.
- Genetic predisposition– Despite practicing rigorous oral hygiene routines, as much as 30% of the population may have a strong genetic predisposition to gum disease. These individuals are six times more likely to develop periodontal disease than individuals with no genetic predisposition. Genetic tests can be used to determine susceptibility and early intervention can be performed to keep the oral cavity healthy.
- Poor dental hygiene– Preventing dental disease starts at home with good oral hygiene and a balanced diet. Prevention also includes regular dental visits which include exams, cleanings, and x-rays. A combination of excellent home care and professional dental care will ensure and preserve the natural dentition and supporting bony structures. When bacteria and calculus (tartar) are not removed, the gums and bone around the teeth become affected by bacteria toxins and can cause gingivitis or periodontitis, which can lead to tooth loss.
- Tobacco use– Research has indicated that smoking and tobacco use is one of the most significant factors in the development and progression of gum disease. In addition to smokers experiencing a slower recovery and healing rate, smokers are far more likely to suffer from calculus (tartar) build up on teeth, deep pockets in the gingival tissue and significant bone loss.
- Pregnancy and menopause– During pregnancy, regular brushing and flossing is critical. Hormonal changes experienced by the body can cause the gum tissue to become more sensitive, rendering them more susceptible to gum disease.
- Grinding teeth– The clenching or grinding of the teeth can significantly damage the supporting tissue surrounding the teeth. Grinding one’s teeth is usually associated with a “bad bite” or the misalignment of the teeth. When an individual is suffering from gum disease, the additional destruction of gingival tissue due to grinding can accelerate the progression of the disease.
Clinical Examination
The periodontal examination gives the dentist a complete picture of the periodontal condition of the patient’s mouth. This information is needed before an accurate diagnosis can be made. The oral exam is supplemented with information gained from the dental X-rays.
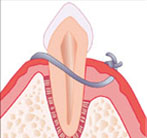
A major focus of the exam is to determine how much bone loss has occurred. When healthy, there is generally a 2-3 millimeter space (sulcus) between the tooth and the gum. This space deepens as bacterial plaque causes bone deterioration, and penetrates down the side of the tooth. This deepened space is called a pocket.
 |
 |
 |
|
Healthy Tooth |
Bone loss leading to pocket formation |
Using a probe to measure pocket depth and bone loss |
Each tooth is measured (probed) (See What is Periodontal Disease?) at six places, surrounding the tooth, to determine the pocket depth. Normally anesthesia is not needed for this charting, which gives the dentist a blueprint of periodontal changes.
 |
 |
|
Probe next to healthy gum |
Probe inserted sulcus bottom (green line measures 3mm) |
 |
 |
|
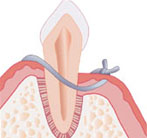
Gum inflammation indicating Periodontal disease |
Probe 5mm into pocket |
Other important information is collected during the examination, so an accurate diagnosis can be made:
- Gum recession – The amount of recession added to the pocket depth determines total bone loss.
- Furcations – Bone loss into the furcation (space between the roots) of a tooth compromises the prognosis.
- Amount of attached gingiva– Without adequate attached gingiva, recession will occur.
- Occlusion (bite) – Excessive forces on teeth may increase the chances of bone loss.
- Tooth mobility (looseness) – Generally indicates inadequate bone support or a bite problem.
- Patient oral hygiene – Poor brushing and flossing will greatly compromise the long-term result.
Dental Radiographs (X-RAYS)
A good series of dental x-rays is mandatory to accurately evaluate periodontal disease. They help determine the amount and location of bone loss, the size and shape of the roots, the amount of root still embedded in bone, the relationship of the teeth to each other, whether the nerve in a tooth has died, the location of the sinus and mandibular nerve when placing implants, and oral pathologies, among other things. We are not able to treat a patient unless we have adequate x-rays. The exception is gingival grafting, which normally does not require x-rays.
There are a number of different types of dental x-rays, each with a specific purpose, but for periodontal treatment a full series of periapical films is generally required. Below is a list of the commonly taken x-ray views, and the indications for each. (Click for a more detailed discussion and examples of each type of x-ray).
- Full Mouth Periapicals – 16 – 18 detailed views of the teeth and surrounding bone, necessary for an accurate periodontal examination.
- Panograph – A single screening film showing an overview of the upper and lower jaws, sinus, temporomandibular joint, and other anatomic features.
- Bitewings – Four detailed views of the side and back teeth, primarily used to detect decay. Often used with the panograph by general dentists for routine new patient screenings.
- Vertical Bitewings – Four to seven detailed views of the teeth that can show both decay and bone levels when severe bone loss has not occurred.
- Digital X-rays – Any x-ray that is stored digitally, on a computer. This further significantly decreases radiation exposure.
Many people have a legitimate concern about the amount of radiation they receive with dental x-rays. It’s un-nerving to watch the technician set the machine and run out of the room to expose the film! However, recent advances in dental x-rays make this an unnecessary concern. The film “speed” has improved dramatically, meaning that very little radiation is needed to expose the film. In fact, it is estimated that the amount of body radiation received with a full mouth series is much less than one would receive at a day at the beach.
Diagnosis
Once the clinical data is gathered and correlated with the x-ray findings, your periodontist is able to organize and systematically evaluate the results to make a diagnosis. This is critical, for while there may be various approaches to treat a problem, there can be only one correct diagnosis. Once the diagnosis is determined, various treatment options can be formulated. With this information the periodontist and the patient can determine which treatment plan to follow.
 |
Treating Periodontal Disease
There are many surgical and nonsurgical treatments the periodontist may choose to perform, depending upon the exact condition of the teeth, gums and jawbone. A complete periodontal exam of the mouth will be done before any treatment is performed or recommended.
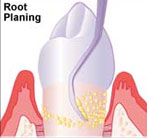
There are two main objectives in treating periodontal disease. The first goal is to reduce and control the bacterial colonies that form under the edge of the gum. The second goal is to eliminate any known factors that cause the patient to be more susceptible to breakdown. Primary among these is smoking. In the early stages of periodontal disease (gingivitis), the gum is infected but the bone has not yet been altered. The pocket depth is generally only slightly deepened; to 4-5 mm.Scaling and root planing(“deep cleanings”) are done to remove any calculus that has formed. If the pockets are tender, numbing the gums is often necessary so there will be no discomfort during the procedure.
Common Treatments for Periodontal Disease
Scaling and Root Planing
In order to preserve the health of the gum tissue, the bacteria and calculus (tartar) which initially caused the infection, must be removed. The gum pockets will be cleaned and treated with antibiotics as necessary to help alleviate the infection. A prescription mouthwash may be incorporated into daily cleaning routines.
There is little or no pain afterward. The patient must keep plaque from reforming by daily brushing and flossing. The healing gum will tighten around the root, and health will return. Daily plaque removal with regular dental cleanings will prevent a reoccurrence.
 |
 |
Pocket Elimination Surgery
In more moderate cases, there is actual bone loss, and the pockets may be 5-7mm in depth. Scaling and root planing will not predictably remove all the calculus from these deeper pockets, because of limited and difficult access in reaching the bottom of the pocket. In these cases flap surgery is needed so the periodontist can gain access to clean the root. With this procedure, an incision is made between the gum and tooth, and the gum is peeled back away from the neck of the tooth and the edge of the bone. The surgeon can then easily see the deep calculus, and adequately debride the tooth.
 |
| Flap reflected to access deep plaque and calculus |
After flap surgery the tissue may be returned to its former position, which minimizes cosmetic changes. However, because the gum cannot connect back to the tooth, this does not eliminate the pocket. With the pocket remaining, the patient cannot remove all the bacteria, and must rely on frequent hygienist cleanings to help control reoccurrence of the infection.
 |
| Flap returned to normal |
The ideal flap surgery, pocket elimination surgery, is achieved when the periodontist surgically removes the pocket by repositioning the gum down to the new bone level. Any irregularities or pitting of the bone that was caused by the infection is first corrected, and the gum is sutured tightly down to the re-contoured bone. This pocket elimination allows the patient to access and remove the bacterial plaque daily with brushing and flossing. If all plaque is eliminated daily, the disease is completely arrested.
Flap Surgery
By far the most common surgery used in periodontal therapy is flap surgery. Moderate to advanced periodontal disease involved gum pockets that are too deep to clean without reflecting back the gum tissue for access. Without this access, deep calculus and plaque cannot be removed from the root, and the disease will progress leading to further bone loss and eventually tooth loss.
 |
 |
| Deep pocket with calculus | Flap reflected to access calculus |
Once the pocket is cleaned, the gum may be returned to its original level.
 |
| A) Gum sutured back to normal height, leaving a deepened space |
This results in a clean root, but the deepened space is still present. Frequent cleanings by the hygienist are necessary to remove the plaque in the residual pocket that the patient cannot reach with flossing and brushing. Even when there is good oral hygiene and regular quarterly recalls, the bacteria may still continue to cause the pocket to become re-infected. When cosmetics are not a concern (on the lower teeth, the inside of the upper teeth, and the outside of the upper back teeth), the surgeon may elect to suture the gum down to where the bone has resorbed, reducing the depth of the space.
 |
| B) Gum sutured down to bone to reduce residual space. |
If the space is reduced to 3 millimeters or less, the patient is able to reach the bottom of the space with daily brushing and flossing, eliminating the disease.
In the majority of advanced cases, the bacteria have caused the bone to resorb and become pitted. In these cases flap surgery gives access not only for root cleansing, but allows for re-contouring of the bone itself. By performing this osseous surgery, and reshaping the bone to its natural scalloped shape, it is generally possible to eliminate moderate pockets. The patient is then able to prevent recurrence of the disease by keeping the shallow space clean with brushing and flossing.
A study was done which compared approach A (replacement of the flap in its original position) with B (placing the flap at the bone crest) after osseous [bone] re-contouring. After 1 year both procedures achieved equal results. After 5 years however, the pockets in group B remained decreased while those in group A recurred. Thus, for long term health it is essential to eliminate bone irregularities. (Olsen, International Journal of Periodontics & Restorative Dentistry 4/1985)
In summary, for most moderate and advanced cases, it is important to be able to reach far under the gum to treat the infection and diseased tissues. By using flap surgery, the periodontist is able to access these areas to provide the optimal care available. With today’s medications, surgery should be painless with only a minimal amount of post-operative discomfort.
 |
 |
| Bone re-contoured after flap reflected.
|
Tissue sutured down to smooth bone to eliminate pocket.
|
 |
 |
| Pitted Bone re-contoured during Osseous surgery | Flap sutured down to re-contour bone |
Pocket elimination surgery can cause cosmetic changes around the upper front teeth, and the periodontist may avoid pocket elimination surgery in this area to minimize any changes that could be seen.
If surgery is necessary, the main scaling and root planing is often done at the surgery, rather than before. During surgery the periodontist can see and reach all areas, allowing for better tooth cleansing. However, each case is treated according to need and in cases where the need for surgery is not certain, the non-surgical scaling and root planing is performed first. The patient is then re-evaluated to see if further treatment is required.
In advanced cases, there has been extensive bone loss, and pocket depth may be 8mm and more. In these cases complete removal of the pocket is often not possible, due to limitations on how far the gum can be moved. However, surgery is necessary for the periodontist to access and clean the deeper areas, which cannot be effectively scaled without reflecting the gum. The objective is to thoroughly cleanse the roots, and to reduce the pockets as much as possible. Antibiotics may be prescribed to help eliminate very aggressive bacteria.
In the last decade there has been much research in actually re-growing the bone destroyed by periodontal disease. While not effective in all cases, today many periodontal lesions can benefit from these regeneration procedures. Your periodontist will tell you if you are a good candidate for regeneration. (See Regeneration)
 |
 |
 |
| Placing substitute bone | Synthetic bone placed in defect | Replacement bone stimulated patient’s natural bone to regenerate |
In cases where surgery is not, or cannot, be performed, or in very advanced cases, there are often residual pockets after treatment. The deeper these pockets, the more guarded the long term results will be. We try to reduce pockets as much as we can. As a rule of thumb, the shallower the pocket, the better the chances of maintaining the tooth. With a shallower pocket the hygienist is able to clean more thoroughly at recall appointments, and the patient is able to remove a greater percentage of the plaque that forms.
Periodontal disease may be considered a chronic disease, and for that reason a complete “cure” is usually not possible. Patient susceptibility may continue to be high, and the cause of infection, plaque, is always present in the mouth. Daily vigilance is needed to control the disease and keep the gums in good health. Even with the best care certain areas may lose ground, although the vast percentage of patients who follow good maintenance can expect to have their teeth for their lifetime.
In summary, the treatment of periodontal disease focuses on removing bacterial plaque and calculus that forms under the gums. In more severe cases surgery is used to provide access for scaling, and to reduce pocket depth so the patient can more effectively access and remove plaque from their teeth at home. Good oral hygiene along with regularperiodontal maintenance appointments (recalls) will help preserve the teeth for a lifetime.
The 3 Steps to Treating Periodontal Disease
The treatment of periodontal disease involves 3 main steps:
- Initial Preparation
- Surgical Treatment
- Maintenance
The following is an overview of the components of each treatment step.
STEP ONE: Initial Preparation
The first step of treatment is to eliminate all of the known causes of the periodontal disease. Mouth bacteria found in saliva forms colonies on the teeth and tissues, which is called plaque. This clear film of bacteria is the primary cause of periodontal inflammation and breakdown. Calculus (also known as tartar) is formed when salts from the saliva precipitate into the plaque. This forms a hard substance, which adheres tightly to the tooth, similar to barnacles on a boat’s hull. Both the calculus and the plaque must be removed to achieve a successful result. The patient is taught to remove the plaque, while the dental professional must remove the calculus. Initial preparation also includes creating an environment that makes plaque removal by the patient as easy as possible. The following outline lists factors that may be addressed during initial preparation.
- Demonstration of proper oral hygiene procedures to remove surface plaque
- Scaling and root planing to remove calculus and deep plaque
- Smoothing or replacement of fillings that do not fit well and thus retain plaque
- Removal of hopeless teeth that may jeopardize good teeth
- Adjustment of bite (occlusal equilibration) if needed
- Minor orthodontics to better align teeth
- Placement of a night guard to prevent clenching at night
Following Initial Preparation, the tissues are re-evaluated after they have a chance to heal to determine if more periodontal therapy is needed. If the disease has been arrested, the optimal periodontal maintenance (cleaning) schedule is determined for the patient. If the disease persists, further non-surgical treatment may be performed. If surgery is needed to eliminate pockets that persist, a surgical treatment plan is formulated.
STEP TWO: Surgical Treatment
Initial Preparation generally produces shrinkage of the inflamed gum, and thus a reduction of the pocket depth. Often, if the patient has excellent oral hygiene habits and keeps regular maintenance appointments, this is enough to stabilize a case.
However, with pockets that continue to bleed when probed, or with pockets deeper than 5mm, there is a high probability the disease process will continue. In those cases elimination of the remaining pockets is the best treatment. If it is obvious during the examination that surgery is needed to obtain the best result, parts of the Initial Preparation may be abbreviated or by-passed completely. Scaling and root planing may be done during surgery, when access is the most ideal. This approach avoids repeating steps of Initial
Preparation that would be performed during surgery, saving time and reducing costs.
There are three primary surgical procedures that may be used to reduce or eliminate pockets that remain after Initial Preparation (Click any heading for a more detailed discussion and clinical examples).
Gingivectomy – Trimming excess tissue when the bone contour has not been altered.
Flap Surgery – The most common surgical procedure, giving the periodontist access to the jawbone. In most advanced periodontal cases, the bone has been altered by infection and smoothing irregularities is needed.
Regeneration Surgery – Ideally, periodontal therapy would regenerate bone and tissue back to its original form. While this is not always possible, new techniques are allowing for more predictable regeneration of tissues.
The goal of periodontal surgery is to give the periodontist access for treatment, and to reduce pocket depth. The ideal surgical result is pocket elimination, giving the patient the ability to remove plaque from the sulcus daily. In some cases the pockets are so deep that complete elimination is not possible, and some depth remains even after surgery. Some of these teeth may be considered questionable, and their long-term prognosis guarded. However, as long as these teeth do not jeopardize surrounding dentition, are functional, and do not cause discomfort, they are maintained. Many questionable teeth are kept for years, if the patient is able to perform a high level of oral hygiene and stay on a good maintenance program.
| 3 month recalls reduce bone loss |  |
At the periodontal maintenance appointment the following procedures are performed:
- Update of medical and dental history
- Soft tissue cancer exam
- Clinical decay examination
- Clinical periodontal examination
- Review of oral hygiene as needed
- Scaling above the gum level
- Root planing under the gum level as needed
- Administration of fluoride as needed
- Polishing
- Doctor check
- Confirmation of recall frequency and scheduling of next appointment
Full mouth radiographs, which show the entire root surface, are taken every 2-3 years to determine if the bone level is stable.
An important observation at a periodontal maintenance appointment is whether the tissues bleed when probed. If there is no bleeding, the mouth is healthy. If there is bleeding, and it is seen on several subsequent recalls, additional treatment in that area is warranted. A change of the bone level as seen on X-rays also requires attention.
The periodontal maintenance appointment should be comfortable and pleasant, and for those patients who need help relaxing, nitrous oxide (“laughing gas”) is available.
It only takes twenty four hours for plaque that is not removed from your teeth to turn into calculus (tartar)! Daily home cleaning helps control plaque and tartar formation, but those hard to reach areas will always need special attention.
Once your periodontal treatment has been completed, your dentist and dental hygienist will recommend that you have regular maintenance cleanings (periodontal cleanings), usually four times a year. At these cleaning appointments, the pocket depths will be carefully checked to ensure that they are healthy. Plaque and calculus that is difficult for you to remove on a daily basis will be removed from above and below the gum line.
In addition to your periodontal cleaning and evaluation, your appointment will usually include:
- Examination of diagnostic x-rays (radiographs): Essential for detection of decay, tumors, cysts, and bone loss. X-rays also help determine tooth and root positions.
- Examination of existing restorations: Check current fillings, crowns, etc.
- Examination of tooth decay: Check all tooth surfaces for decay.
- Oral cancer screening: Check the face, neck, lips, tongue, throat, cheek tissues, and gums for any signs of oral cancer.
- Oral hygiene recommendations: Review and recommend oral hygiene aids as needed. (Electric toothbrushes, special periodontal brushes, fluorides, rinses, etc.)
- Teeth polishing: Remove stain and plaque that is not otherwise removed during tooth brushing and scaling.
Good oral hygiene practices and periodontal cleanings are essential in maintaining dental health and keeping periodontal disease under control!
The Patient’s Role
Home Care
Mouth Body Connection
No matter how successful the periodontal treatment has been, the patient is the most important part in maintaining periodontal health. For maximum results, the patient must accept this role as a “co-therapist”.
The first charge to the patient is to eliminate factors that increase susceptibility to periodontal disease. The prime culprit is smoking, which increases the odds of losing teeth. Diabetic patients are also more susceptible, although this effect is negligible if the blood sugar remains stable. Healthy diets promote healing, but don’t be misled by vitamin claims. Periodontal disease is NOT affected by high doses of Vitamin C or calcium supplements, if the patient has a normal diet.
The second responsibility of the patient is to maintain daily plaque control, with brushing and flossing. Brushing is easy for most of us, but flossing is more demanding. Most periodontal disease, however, starts between the teeth, where the brush cannot reach. “Floss is Boss”, and the time spent in learning proper technique will pay large dividends. (See Oral Hygiene)
Lastly, the patient is responsible for scheduling regular periodontal maintenance. The frequency is determined by your periodontist and dentist, and is critical! Most patients with moderate and advanced cases should have periodontal maintenance appointments every three months for their lifetime, and staying faithful to this schedule is very important (See Periodontal Maintenance).
Home Care
A beautiful, healthy smile that lasts a lifetime is our ultimate goal when treating patients. Your personal home care is the MOST IMPORTANT in achieving that goal. Your personal home care starts by eating balanced meals, reducing the number of snacks you eat, and correctly using the various dental aids that help control the plaque and bacteria that cause dental disease.
Tooth brushing
Brush your teeth at least twice a day (especially before going to bed at night) with an ADA approved soft bristle brush and toothpaste.
- Place the brush at a 45 degree angle to the gums and gently brush using a small, circular motion, ensuring that you always feel the bristles on the gums.
- Brush the outer, inner, and biting surfaces of each tooth.
- Use the tip of the brush to clean the inside of the front teeth.
- Brush your tongue to remove bacteria and freshen your breath.
Brushing time should be a minimum of 3 minutes per session. When brushing your teeth, don’t think of it as scrubbing a floor, but as detailing an automobile.
 |
 |
 |
| Brush angles under the gum
|
Brushing lower molars
|
Brushing upper molars
|
Electric toothbrushes are also recommended. They are easy to use and can remove plaque efficiently. New models that can oscillate and pulsate the brush head 40,000 times/min are far superior than conventional manual brushing. Simply place the bristles of the electric brush on your gums and teeth and allow the brush to do its job, several teeth at a time. Many electric toothbrushes have timer features built in, letting you know when you brushed for an adequate amount of time.
Flossing
Daily flossing is the best way to clean between the teeth and under the gum line. Flossing not only helps clean these spaces, it disrupts plaque colonies from building up, preventing damage to the gums, teeth, and bone.
 |
 |
| Floss between teeth, but not yet under gum | Floss wrapped under gum
|
- Take 12-16 inches (30-40cm) of dental floss and wrap it around your middle fingers, leaving about 2 inches (5cm) of floss between the hands.
- Using your thumbs and forefingers to guide the floss, gently insert the floss between teeth using a sawing motion.
- Curve the floss into a “C” shape around each tooth and under the gum line. Gently move the floss up and down, cleaning the side of each tooth.
Many patients don’t realize that flossing is more important than brushing. The areas between teeth are more plaque retentive – tooth decay and gingivitis generally develop between the teeth first!
Floss holders are recommended if you have difficulty using conventional floss.
Order of Hygiene:
- Brush in the morning (preferably after breakfast) for a minimum of 3 minutes
- Evening (immediately before bedtime) – floss, rinse and then brush
*Use other dental aids as recommended by your dentist or dental hygienist: Interdental brushes, rubber tip stimulators, tongue cleaners, irrigation devices, fluoride, medicated rinses, etc., can all play a role in good dental home care.
There are many other aids that are available to help with oral hygiene. These include small brushes that can clean spaces between the teeth (proxibrush), and threaders to guide floss under bridges (floss threaders). Toothpicks may be recommended to help clean furcations. Each patient is individually assessed to see what may help optimize their cleaning efforts.
 |
 |
| Proxibrush entering space between teeth | Proxibrush cleaning between teeth |
Mouth – Body Connection
Diabetes
Heart Disease & Stroke
Pregnancy Complications
- Respiratory Disease
- Osteoporosis
Research studies have shown that there is a strong association between periodontal disease and other chronic conditions such as diabetes, heart disease, pregnancy complications and respiratory disease.
Periodontal disease is characterized by chronic inflammation of the gum tissue, periodontal infection below the gum line and a presence of disease-causing bacteria in the oral region. Halting the progression of periodontal disease and maintaining excellent standards of oral hygiene will not only reduce the risk of gum disease and bone loss, but also reduce the chances of developing other serious illnesses.
Common co factors associated with periodontal disease:
Diabetes
A research study has shown that individuals with pre-existing diabetic conditions are more likely to either have, or be more susceptible to periodontal disease. Periodontal disease can increase blood sugar levels which makes controlling the amount of glucose in the blood difficult. This factor alone can increase the risk of serious diabetic complications. Conversely, diabetes thickens blood vessels and therefore makes it harder for the mouth to rid itself of excess sugar. Excess sugar in the mouth creates a breeding ground for the types of oral bacteria that cause gum disease.
It is well documented that people who suffer from diabetes are more susceptible to developing infections than non-diabetes sufferers. It is not widely known that t periodontal disease is often considered the sixth complication of diabetes; particularly when the diabetes is not under proper control.
Periodontal disease (often called periodontitis and gum disease) is a progressive condition that often leads to tooth loss if treatment is not promptly sought. Periodontal disease begins with a bacterial infection in the gingival tissue which surrounds the teeth. As the bacteria colonize, the gum pockets become deeper, the gums recede as tissue is destroyed and the periodontitis eventually attacks the underlying bone tissue.
Diabetes is characterized by too much glucose (or sugar) in the blood. Type II diabetics are unable to regulate insulin levels which means excess glucose stays in the blood. Type I diabetics do not produce any insulin at all. Diabetes is a serious condition which can lead to heart disease and stroke.
Reasons for the Connection
Experts suggest the relationship between diabetes and periodontal disease can worsen both conditions if either condition is not properly controlled.
Here are ways in which diabetes and periodontal disease are linked:
Increased blood sugar– Moderate and severe periodontal disease elevates sugar levels in the body, increasing the amount of time the body has to function with high blood sugar. This is why diabetics with periodontitis have difficulty keeping control of their blood sugar. In addition, the higher sugar levels found in the mouth of diabetics provide food for the very bacteria that worsen periodontal infections.
Blood vessel thickening– The thickening of the blood vessels is one of the other major concerns for diabetes sufferers. The blood vessels normally serve a vital function for tissues by delivering nutrients and removing waste products. With diabetes, the blood vessels become too thick for these exchanges to occur. This means that harmful waste is left in the mouth and can weaken the resistance of gum tissue, which can lead to infection and gum disease.
Smoking – Tobacco use does a great deal of damage in the oral region. Not only does tobacco use slow the healing process, it also vastly increases the chances of an individual developing periodontal disease. For diabetics who smoke, the risk is exponentially greater. In fact, diabetic smokers aged 45 and over are twenty times more likely to develop periodontal disease.
Poor oral hygiene– It is essential for diabetics to maintain excellent levels of oral health. When daily brushing and flossing does not occur, the harmful oral bacteria can ingest the excess sugar between the teeth and colonize more freely below the gum line. This exacerbates the metabolic problems that diabetes sufferers experience.
Diagnosis and Treatment
It is of paramount importance for people suffering from any type of diabetes to see the dentist at least twice yearly for checkups and professional cleanings. Studies have shown that simple non-surgical periodontal treatments can lower the HbA1c (hemoglobin molecule blood test) count by as much as 20% in a six month period.
The dentist will use medical history, family history and dental X-rays to assess the risk factors for periodontal disease and determine the exact condition of the gums, teeth and underlying jawbone. If necessary the dentist will work in conjunction with other doctors to ensure that both the diabetes and the gum disease are being managed and controlled as effectively as possible.
Non-surgical procedures performed by the dentist and dental hygienist include deep scaling, where calculus (tartar) will be removed from the teeth above and below the gumline, and root planing, where the root of the tooth is smoothed down to eliminate any remaining bacteria. Antibiotics may be applied to the gum pockets to promote healing.
Before and after periodontal treatment, the dentist and hygienist will recommend proper home care and oral maintenance as well as prescribing prescription mouthwashes which serve to deter further bacteria colonization.
If you have questions or concerns about diabetes or periodontal disease, please ask your dentist.
Heart Disease & Stroke
There are several theories which explain the link between heart disease and periodontitis. One such theory is that the oral bacteria strains which exacerbate periodontal disease attach themselves to the coronary arteries when they enter the bloodstream. This in turn contributes to both blood clot formation and the narrowing of the coronary arteries, possibly leading to a heart attack.
A second possibility is that the inflammation caused by periodontal disease causes a significant plaque buildup. This can swell the arteries and worsen pre-existing heart conditions. An article published by the American Academy of Periodontology suggests that patients whose bodies react to periodontal bacteria have an increased risk of developing heart disease.
Periodontal disease, heart disease and stroke may seem to be unlikely bedfellows, but researchers have found that gum disease sufferers are nearly twice as likely to also suffer from coronary heart disease. In addition, research studies have discovered that oral infection is indeed a risk factor for stroke. People diagnosed with acute cerebrovascular ischemia were more likely to also be experiencing some degree of periodontal disease.
Periodontal disease is a progressive condition in which the gingival tissue surrounding the teeth is infected by the colonization of bacteria. Bacteria found in plaque colonize first above, then below the gum line causing the tissue to pull away from the teeth. If periodontal disease is left untreated, deep pockets form between the gums and the teeth and the tissue of the underlying jawbone is also destroyed. The destruction of bone tissue causes the teeth to shift, wobble or completely detach from the bone.
Coronary heart disease occurs when the walls of the coronary arteries become progressively thicker due to the buildup of fatty proteins. The heart then suffers from a lack of oxygen and must labor significantly harder to pump blood to the rest of the body. Coronary heart disease sufferers sometimes experience blood clots which obstruct normal blood flow and reduce the amount of vital nutrients and oxygen the heart needs to function properly. This phenomenon often leads to heart attacks.
Reasons for the Connection
There is little doubt that the presence of periodontal disease can exacerbate existing heart conditions. The periodontist and cardiologist generally work as a team in order to treat individuals experiencing both conditions.
There are several theories which may explain the link between heart disease, stroke and periodontal disease, which include the following:
Oral bacteria affect the heart– There are many different strains of periodontal bacteria. Researchers assert that some of these strains of bacteria enter the bloodstream and attach to the fatty plaques in the heart blood vessels (coronary arteries). This attachment then contributes to clot formation causing grave danger to the individual.
Inflammation– Periodontal disease causes severe inflammation in the gum tissue which elevates the white blood cell count and also the high sensitivity C-reactive protein levels. Research studies have shown that elevated levels of C-reactive proteins have been linked to heart disease.
Infectious susceptibility– Individuals who experience particularly high levels of oral bacteria may have weaker immune systems and an inadequate host inflammatory response. These factors may induce specific vascular effects which have previously been shown to contribute in the onset of certain forms of heart disease.
Diagnosis and Treatment
Since periodontal disease appears to be a risk factor for both heart attack and stroke, it is extremely important to seek immediate treatment. Initially, the periodontist will conduct thorough examinations to assess the exact condition of the teeth, gums and jawbone. X-rays can be helpful in determining whether bone loss is prevalent in the upper and lower jaw.
The dentist is able to conduct deep cleaning treatments such as scaling and root planing to remove hardened calculus (tartar) deposits from the gum pockets. An antibiotic may be prescribed to ensure that the bacterium is completely destroyed and the periodontal infection does not spread. In most cases, periodontal disease can be prevented with regular cleanings and proper home care.
If you have questions or concerns about periodontal disease and its relation to heart disease and stroke, please ask your dentist.
Pregnancy Complications
Women in general are at increased risk of developing periodontal disease because of hormone fluctuations that occur during puberty, pregnancy and menopause. Research suggests that pregnant women suffering from periodontal disease are more at risk of preeclampsia and delivering underweight, premature babies.
Periodontitis increases levels of prostaglandin, which is one of the labor-inducing chemicals. Elevated levels prostaglandin may trigger premature labor, and increase the chances of delivering an underweight baby. Periodontal disease also elevates C-reactive proteins (which have previously been linked to heart disease). Heightened levels of these proteins can amplify the inflammatory response of the body and increase the chances of preeclampsia and low birth weight babies.
Researchers have shown that periodontal disease in expectant mothers actually exposes their unborn child to many different risks; particularly if they also happen to be diabetes sufferers.
Periodontal disease generally begins with a bacterial infection in the gum (gingival) tissue, which progressively destroys the tissue and the underlying bone. If left untreated, the bacterial infection causes an inflammatory reaction in the body, which can significantly deepen the gum pockets (space between the teeth and gums) and forces the gum and jawbone to recede. Eventually, the progressive nature of periodontal disease causes the teeth to become loose and unstable, and eventually fall out.
Pregnancy causes many hormonal changes which increase the risk of the expectant mother to develop gingivitis (inflammation of the gum tissue) and periodontal disease. These oral problems have been linked in many research studies to preeclampsia, low birth weight of the baby and premature birth. Expectant women should seek immediate treatment for periodontal disease in order to reduce the risk of pre-natal and post-natal complications.
Reasons for the Connection
There are many different reasons why periodontal disease may affect the health of the mother and her unborn child:
Prostaglandin – Periodontal disease appears to elevate levels of prostaglandin in mothers who are suffering from the more advanced forms of the condition. Prostaglandin is a labor-inducing compound found in one of the oral bacteria strains associated with periodontitis. Elevated levels of prostaglandin can cause the mother to give birth prematurely and deliver a baby with a low birth weight.
C – reactive protein (CRP) – This protein, which has been previously linked to heart disease, has now been associated with adverse pregnancy outcomes including preeclampsia and premature birth. Periodontal infections elevate C-reactive protein levels and amplify the body’s natural inflammatory response. Periodontal bacteria may enter the bloodstream causing the liver to produce CRP which leads to inflamed arteries as well as possible blood clots. These inflammatory effects can then lead to blocked arteries causing strokes or heart attacks.
Bacteria spread– The bacteria which colonize in the gum pockets can readily travel through the bloodstream and affect other parts of the body. In pregnant women, research has found that oral bacteria and associated pathogens have colonized in the internal mammary glands and coronary arteries.
Diagnosis and Treatment
There are many safe, non-surgical treatment options available for pregnant women. It is of paramount importance to halt the progress of periodontal disease in order to increase the chances of a safe and healthy delivery.
Initially, the dentist will assess the exact condition of the gums and jawbone in order to make a precise diagnosis. Scaling and root planing are two common non-surgical procedures used to rid the tooth-root surfaces of calculus (tartar) and remove the bacterial toxins from the gum pockets.
The advantages to the pregnant woman are plentiful. The risks of pregnancy complications caused by periodontal disease are reduced by as much as 50%, and these treatments will alleviate many unpleasant and harmful effects associated with gingivitis and periodontal infection.
Dentists can provide dental education and recommendations to the pregnant women on effective home care which can reduce risks that may affect her and/or her child’s health. Risks of periodontal disease can be vastly reduced by proper home care, smoking cessation, dietary changes and the ingestion of supplementary vitamins.
It is recommended that pregnant women have professional cleanings at least every 2-3 months.
If you have any questions or concerns about periodontal disease and its effect on pregnancy, please ask your dentist.
Respiratory Disease
Oral bacterium linked with gum disease has been shown to possibly cause or worsen conditions such as emphysema, pneumonia and Chronic Obstructive Pulmonary Disease (COPD). Oral bacteria can be drawn into the lower respiratory tract during the course of normal inhalation and colonize; causing bacterial infections. Studies have shown that the repeated infections which characterize COPD may be linked with periodontitis.
In addition to the bacterial risk, inflammation in gum tissue can lead to severe inflammation in the lining of the lungs, which aggravates pneumonia. Individuals who suffer from chronic or persistent respiratory issues generally have low immunity. This means that bacteria can readily colonize beneath the gum line unchallenged by body’s immune system.
Periodontal disease (also called periodontitis and gum disease) has been linked to respiratory disease through recent research studies. Researchers have concluded that periodontal disease can worsen conditions such as chronic obstructive pulmonary disease (COPD) and may actually play a causal role in the contraction of pneumonia, bronchitis and emphysema.
Periodontal disease is a progressive condition which generally begins with a bacterial infection. The bacteria found in plaque begin to colonize in gingival tissue, causing an inflammatory response in which the body destroys both gum and bone tissue. The sufferer may notice the teeth “lengthening” as the gums recede while the disease progresses. If left untreated, erosion of the bone tissue brings about a less stable base for the teeth, meaning loose, shifting or complete tooth loss.
There are a number of different respiratory diseases linked to periodontal disease. Pneumonia, COPD, and bronchitis are among the most common. Generally, bacterial respiratory infections occur due to the inhalation of fine droplets from the mouth into the lungs. COPD is a leading cause of death and should be taken very seriously.
Diagnosis and Treatment
When respiratory disease and periodontal disease are both diagnosed in one individual, it is important for the dentist and doctor to function as a team to control both conditions. There are many non-surgical and surgical options available, depending on the specific condition of the teeth, gums and jaw.
The dentist is able to assess the extent of the inflammation and tissue loss and can treat the bacterial infection easily. Scaling procedures cleanse the pockets of debris and root planing smoothes the tooth root to eliminate any remaining bacteria. The dentist generally places antibiotics into the pockets after cleaning to promote good healing and reduce the risk of the infection returning.
Whichever treatment is deemed the most suitable, the benefits of controlling periodontal disease are two-fold. Firstly, any discomfort in the oral region will be reduced and the gums will be much healthier. Secondly, the frequent, unpleasant respiratory infections associated with COPD and other common respiratory problems will reduce in number.
If you have questions or concerns about respiratory disease or periodontal disease, please ask your dentist
Osteoporosis
Periodontal disease is characterized by a progressive loss of supportive gingival tissue in the gums and jawbone. It is the number one cause of tooth loss among adults in the developed world. Periodontal disease occurs when toxins found in oral plaque inflame and irritate the soft tissues surrounding the teeth. If left untreated, bacteria colonies initially cause the systematic destruction of gum tissue, and then proceed to destroy the underlying bone tissue.
Osteoporosis is a common metabolic bone disease which frequently occurs in postmenopausal women, and occurs less frequently in men. Osteoporosis is characterized by bone fragility, low bone mass and a decrease in bone mineral density. Many studies have explored and identified a connection between periodontal disease and osteoporosis.
A study conducted at the University of New York at Buffalo in 1995 concluded that post-menopausal women who suffered from osteoporosis were 86% more likely to also develop periodontal disease.
Reasons for the Connection
Though studies are still being conducted in order to further assess the extent of the relationship between osteoporosis and periodontal disease, the researchers have thus far made the following connections:
Estrogen deficiency– Estrogen deficiency accompanies menopause and also speeds up the progression of oral bone loss. The lack of estrogen accelerates the rate of attachment loss (fibers and tissues which keep the teeth stable are destroyed).
Low mineral bone density– This is thought to be one of several causes of osteoporosis, and the inflammation from periodontal disease makes weakened bones more prone to break down. This is why periodontitis can be more progressive in patients with osteoporosis.
Diagnosis and Treatment
Osteoporosis and periodontal disease are much less dangerous if they are diagnosed in the early stages. Once a diagnosis has been made, the dentist will generally work with the patient’s doctor to ensure that both diseases are effectively controlled.
Here are some methods commonly used to diagnose and treat the diseases:
Routine dental x-rays– X-rays can be effectively used to screen for bone loss in the upper and lower jaw, and the dentist can provide interventions for preventing and treating periodontal disease. It is believed that minimizing periodontal disease will help treat osteoporosis.
Estrogen supplements– Providing post-menopausal women with estrogen supplements lowers the rate of attachment loss and also lowers gingival inflammation, which in turn protects the teeth from periodontal disease.
Reasons for the Connection
The fact that respiratory disease and periodontal disease are linked may seem far-fetched, but there is plenty of evidence to support it.
Here are some of the reasons for the link between periodontal disease and respiratory disease:
Bacterial spread– The specific type of oral bacterium that causes periodontal disease can easily be drawn into the lower respiratory tract. Once the bacteria colonize in the lungs, it can cause pneumonia and exacerbate serious conditions such as COPD.
Low immunity– It has been well-documented that most people who experience chronic or persistent respiratory problems suffer from low immunity. This low immunity allows oral bacteria to embed itself above and below the gum line without being challenged by the body’s immune system. Not only does this accelerate the progression of periodontal disease, it also puts the sufferer at increased risk of developing emphysema, pneumonia and COPD.
Modifiable factors – Smoking is thought to be the leading cause of COPD and other chronic respiratory conditions. Tobacco use also damages the gingiva and compromises the good health of the oral cavity in its entirety. Tobacco use slows the healing process, causes gum pockets to grow deeper and also accelerates attachment loss. Smoking is not the sole cause of periodontal disease, but it is certainly a cofactor to avoid.
Inflammation – Periodontal disease causes the inflammation and irritation of oral tissue. It is possible that the oral bacteria causing the irritation could contribute to inflammation of the lung lining, thus limiting the amount of air that can freely pass to and from the lungs.
Assessment of risk factors– Dentists and doctors are able to closely monitor the patients that are at an increased risk of developing both diseases by assessing family history, medical history, X-ray results, current medications and modifiable risk factors. Tobacco use, obesity, poor diet and estrogen deficiency can all be managed using a combination of education, support and prescription medications.
If you have any questions about periodontal disease and its connection with osteoporosis, please ask your dentist.
What to Expect from Surgery
Years ago periodontal surgery was considered an ordeal. Things have changed! Today there should be no pain involved during surgery, and the postoperative discomfort is minimal. New and sophisticated medications ensure you a smooth procedure.
Some patients may prefer to be sedated during surgery. With sedation, an hour procedure seems like 5 minutes, and you are not even aware of the local anesthetic when it is given. Of all the additions to modern periodontics, this is the most significant for patient comfort. If sedation is used, you must have a driver. If your driver does not stay for the surgery, he/she must be back 15 minutes before the scheduled appointment end. Please discuss this prior to your surgery with the dentist if you are interested.
Postoperative discomfort has been dramatically reduced with the use of NSAIDS (non-steroid anti-inflammatory drugs). These drugs, such as naprosyn and ibuprofen, stop the formation of the chemicals the body normally produces that cause heightened pain. NSAIDS are not narcotics, so you can function normally when taking them. Generally, NSAIDS are started just after the surgery, and taken for three days. After this time no prescription medications are normally needed. In addition to the NSAIDS, a narcotic is often recommended for the first day. It is used along with the NSAID, and will eliminate any “breakthrough” discomfort. Generally these medications are not needed more than the first day, if at all.
Some patients, particularly those receiving implant or regenerative therapy, are given antibiotics to take after surgery. It is important to take the prescriptions as directed, in order to optimize healing.
A prescription mouthwash is often prescribed after surgery, and may be used for 2-10 weeks. It is much more effective than any over-the-counter mouthwash, and kills bacteria throughout the mouth. During the first 10 days there is generally a periodontal dressing over the operated area (similar to putty or chewing gum), and using the mouthwash keeps the dressing clean.
At 7-14 days any dressing is removed, along with sutures that may have been placed. The area is cleansed, and postoperative care of the area reviewed. This appointment generally lasts 15-30 minutes, and should not cause discomfort.
With most cases it is important to keep all bacteria away from the surgical site for 8-10 weeks. To help ensure optimal plaque control, polish appointments are often scheduled every 2-3 weeks. The prescription mouthwash may also be continued during this time. We have found that careful control of plaque during the healing phase greatly enhances surgical results.